
Book a Consultation
Thank you!
Your form has been sent successfully.



September 14, 2023
Anal cancer is a rare form of cancer that requires immediate attention once detected. According to the American Cancer Society*, approximately 9,760 new anal cancer cases will be diagnosed in 2023. Anal cancer is mostly curable when diagnosed and treated early before cancer metastasizes and spreads to distant organs.
In this blog, we will share detailed insights into the surgical procedures for anal cancer treatment. Read on to find out more.
The primary course of treatment for anal cancer usually involves a combination of chemotherapy and targeted radiation treatment. Nevertheless, in some cases, healthcare providers may consider surgical intervention to eliminate small tumors that have not metastasized to nearby organs or the sphincter muscles. The following are some cases where oncologists usually recommend surgery for anal cancer treatment.
In the initial stages of anal cancer, healthcare providers recommend surgery to remove the cancerous tumor before it spreads to nearby lymph nodes or other organs.
In more advanced cases where the tumor has grown larger or invaded nearby structures, a more extensive surgical approach may be necessary. In such cases, doctors may recommend abdominoperineal resection (APR) or pelvic exenteration.
These surgical interventions are complex and usually combined with other treatments like chemotherapy or radiation therapy for a better prognosis.
In some situations where anal cancer has metastasized and spread to distant organs or when the tumor is inoperable due to its location or size, healthcare providers usually avoid surgical interventions. However, palliative surgery can still play a crucial role in relieving symptoms and enhancing the quality of life.
For instance, healthcare professionals may recommend surgeries to address bleeding, blockages, or pain caused by the tumor.
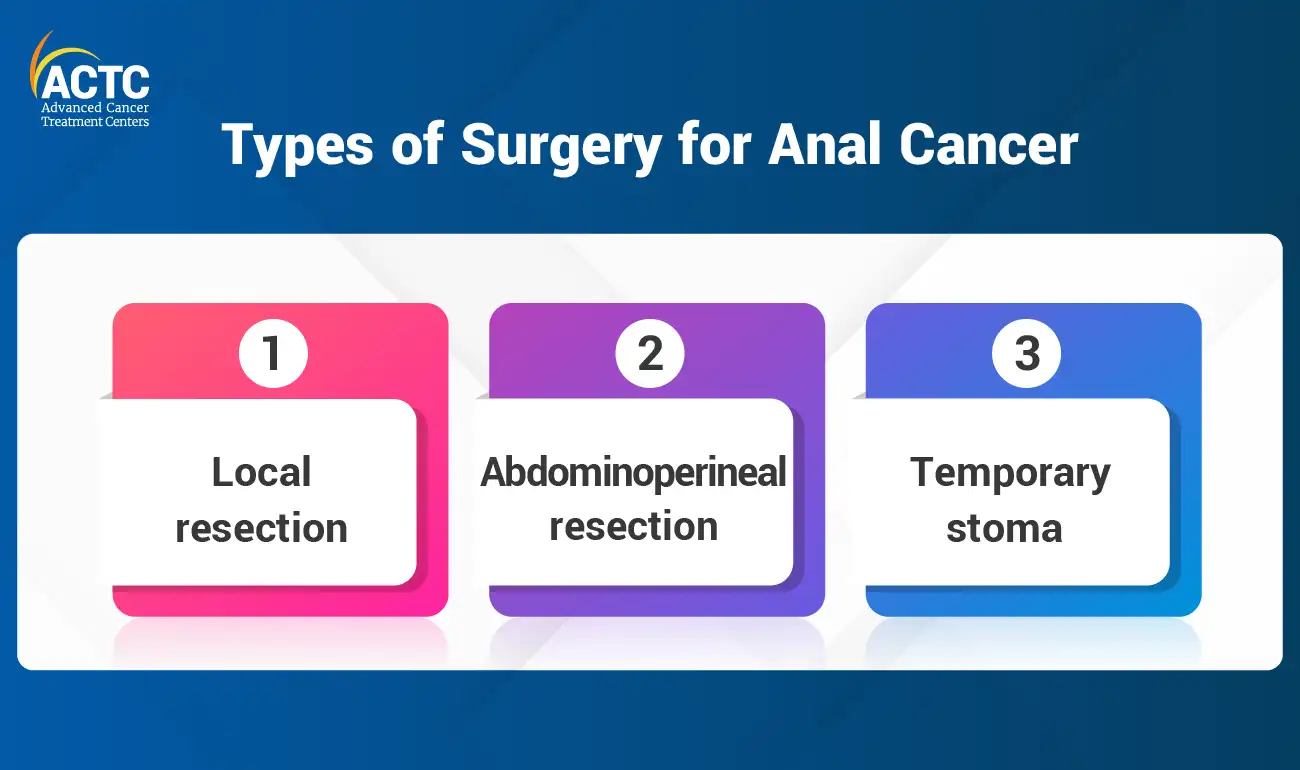
Also known as local excision, local resection is a less invasive surgical procedure primarily recommended by oncologists for early-stage anal cancer. In this procedure, the surgeon removes the cancerous tumor along with a small margin of healthy tissue surrounding it.
This technique has shown effective results for small tumors that have not yet invaded nearby organs or lymph nodes. Local resection can be done only in those cases where tumors are easily accessible and confined to the surface layers of the anal region.
Cancer care specialists recommend abdominoperineal resection (APR) in more advanced cases. In this invasive procedure, surgeons remove the anus, rectum, and part of the sigmoid colon. They may even consider removing nearby lymph nodes if they are affected by cancer.
Following an APR, the surgeon creates a permanent colostomy, a surgical opening on the abdomen through which stool is diverted into a colostomy bag. Although the idea of a permanent colostomy can be frightening, modern colostomy bags are discreet and can significantly improve an individual’s quality of life.
In some cases, especially where the tumor is located in the lower part of the rectum or anal canal, oncologists may consider a temporary stoma. This process involves creating a temporary surgical opening on the abdomen to divert the fecal stream away from the affected area.
A temporary stoma allows the surgical site to heal properly after a major procedure like APR. Once healing is complete, the stoma is reversed, and bowel function is restored to a more natural state.
The main goal of surgery for anal cancer is to remove the cancerous growths and prevent the disease from invading further into the other organs. Additionally, surgical procedures are important in cases where chemotherapy and radiation therapy may not provide sufficient results. Everyone's treatment plan is unique, and the decision to undergo surgery depends on several factors. Individuals should discuss their options with their healthcare team about the available surgical options and potential outcomes.
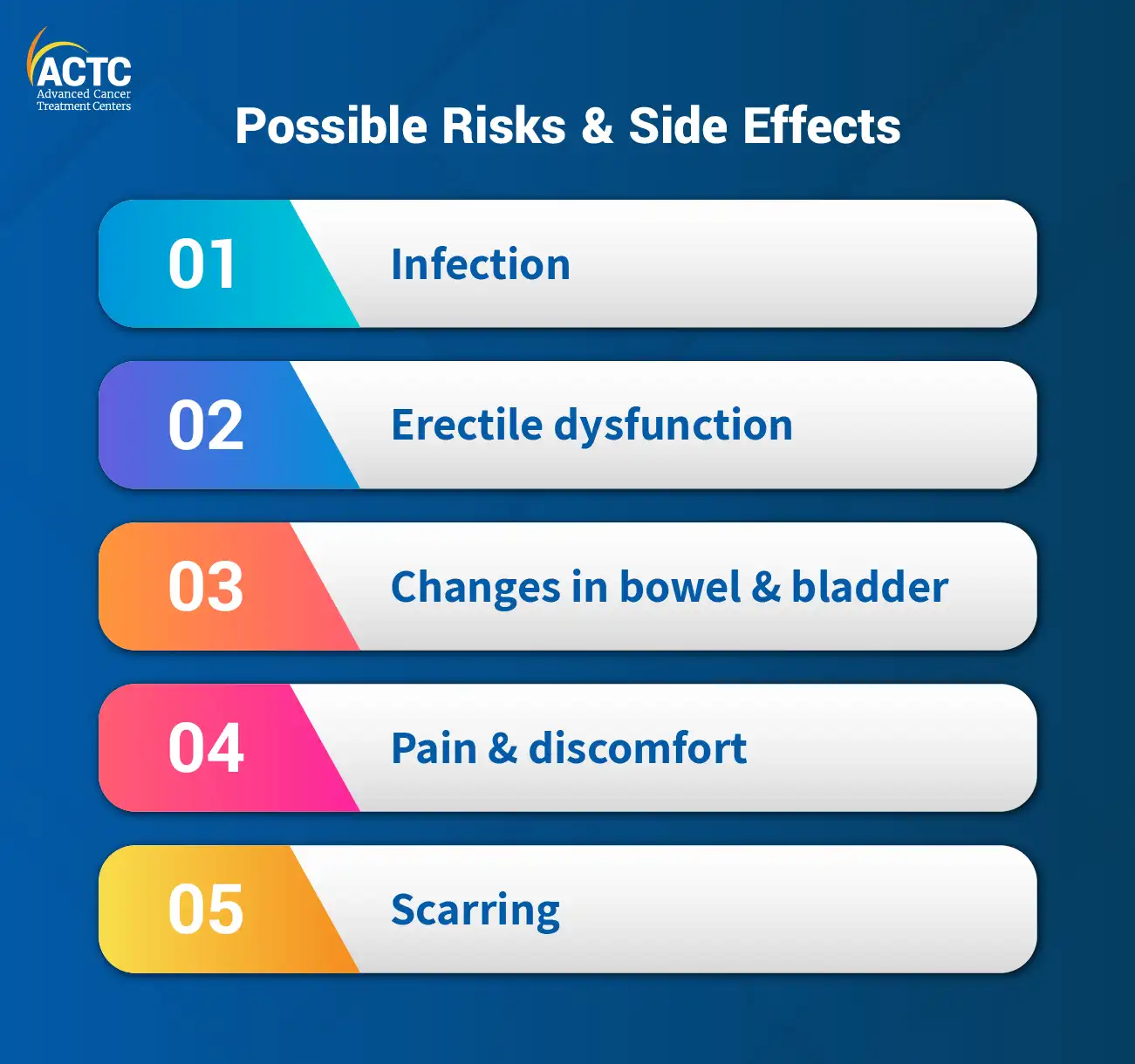
Like any other treatment procedure, surgery also comes with some risks and side effects, which are as follows:
Surgical procedures involve the risk of infection at the site of incision or in the surrounding areas. Doctors may prescribe antibiotics to prevent wound infections. Individuals should consult a doctor immediately if they notice increased heat around the wound area, intensifying pain, uncontrolled bleeding, or any discharge or leakage of fluids from the wound site.
Individuals may experience temporary or permanent changes in bowel and bladder function, especially in the case of permanent colostomy and temporary stoma. Consult a healthcare professional to get detailed guidance on how to cope with these conditions more effectively.
Read more: All You Need to Know About Bladder Cancer
If the surgical procedures involve the removal of the rectum, anus, and nearby structures, it can affect the nerves and blood vessels responsible for erectile function in men. It is possible to manage these changes through medication, counseling, and therapies, as recommended by a healthcare professional.
It is common to experience temporary pain and discomfort in the surgical area, which is manageable with medication and non-pharmacological interventions.
Surgery leaves scars, and the extent of scarring depends on the type of procedure performed. Modern surgical techniques aim to minimize scarring. However, individuals can discuss with their healthcare provider about minimizing scarring or opt for counseling if they feel self-conscious about their appearance.
Individuals should discuss potential risks and side effects with their healthcare team before undergoing surgery. It is best to contact a specialized cancer treatment center, where a multidisciplinary team will collaborate to provide comprehensive cancer care and support.
Post surgery, those with a colostomy bag may have difficulty adjusting to the new reality. Individuals with a colostomy bag may need to avoid certain gas-inducing foods, including high-fiber fruits and vegetables, onions, cabbage, fizzy drinks, and fatty foods.
Despite successful surgery and regular follow-up check-ups, there is a possibility of cancer recurrence. According to the studies, the overall recurrence rate for anal cancer is 19% in the United States. If individuals notice unusual health issues or anal cancer symptoms, it is crucial to seek immediate medical attention. In case of recurrence, individuals may have to go through additional surgery, radiation therapy, chemotherapy, or a combination of treatments to target recurrent cancer cells.
For any questions or concerns about anal cancer, contact the Advanced Cancer Treatment Centers. We are one of the leading Florida cancer centers that offer personalized cancer treatment plans under the guidance of a multidisciplinary cancer care team.
*Key statistics for anal Cancer. (n.d.). American Cancer Society.


December 24, 2025
It's natural to wonder if testosterone replacement therapy (TRT) is sa...
KNOW MORE

December 24, 2025
A rash that will not calm down is scary, especially when it changes or...
KNOW MORE
December 24, 2025
Florida’s lung cancer burden remains significant and affects many fa...
KNOW MORE

December 24, 2025
A partial hysterectomy, also called a supracervical hysterectomy, is s...
KNOW MORE

December 24, 2025
Finding a rash on your breast can be unsettling, but remember, many ra...
KNOW MORE
December 16, 2025
Hearing a HER2 gene mutation on a report can feel scary, but it also p...
KNOW MORE
