
Book a Consultation
Thank you!
Your form has been sent successfully.



February 21, 2024
Breast cancer is a widespread health issue that impacts millions of women globally. It is projected that one in eight women in the United States alone experience invasive breast cancer at some point in their lives.
However, early detection using breast tumor tests and treatment greatly improves the prognosis for breast cancer. This emphasizes how very important routine screenings for breast cancer are.
Breast cancer screening involves the use of various medical tests to detect breast cancer in its early stages, often before symptoms manifest.
The primary screening modalities include mammography, clinical breast exams, and breast self-exams.
Mammography:
The most popular method for screening for breast cancer is mammography. It creates finely detailed images of the breast tissue using low-dose X-rays, making it possible for medical professionals to spot anomalies like tumors or microcalcifications.
Women with an average risk of breast cancer are advised to start yearly mammograms at age 40. Individual screening recommendations, however, might change depending on things like personal health history and family history.
Clinical Breast Exams (CBE):
Clinical breast exams involve a healthcare provider manually examining the breasts for any lumps, irregularities, or changes in texture or appearance.
While not as sensitive as mammography, clinical breast tumor tests can still help in the early detection of breast cancer, particularly when performed along with other screening methods.
Breast Self-Exams (BSE):
Breast self-exams empower women to become familiar with their own breast tissue and detect any changes that may warrant further evaluation. While BSEs are no longer recommended as a standalone screening method due to concerns regarding their efficacy, they can still complement regular mammograms and clinical breast exams.
Understanding the risk factors associated with breast cancer is crucial for identifying individuals who may benefit from more frequent or intensive screening.
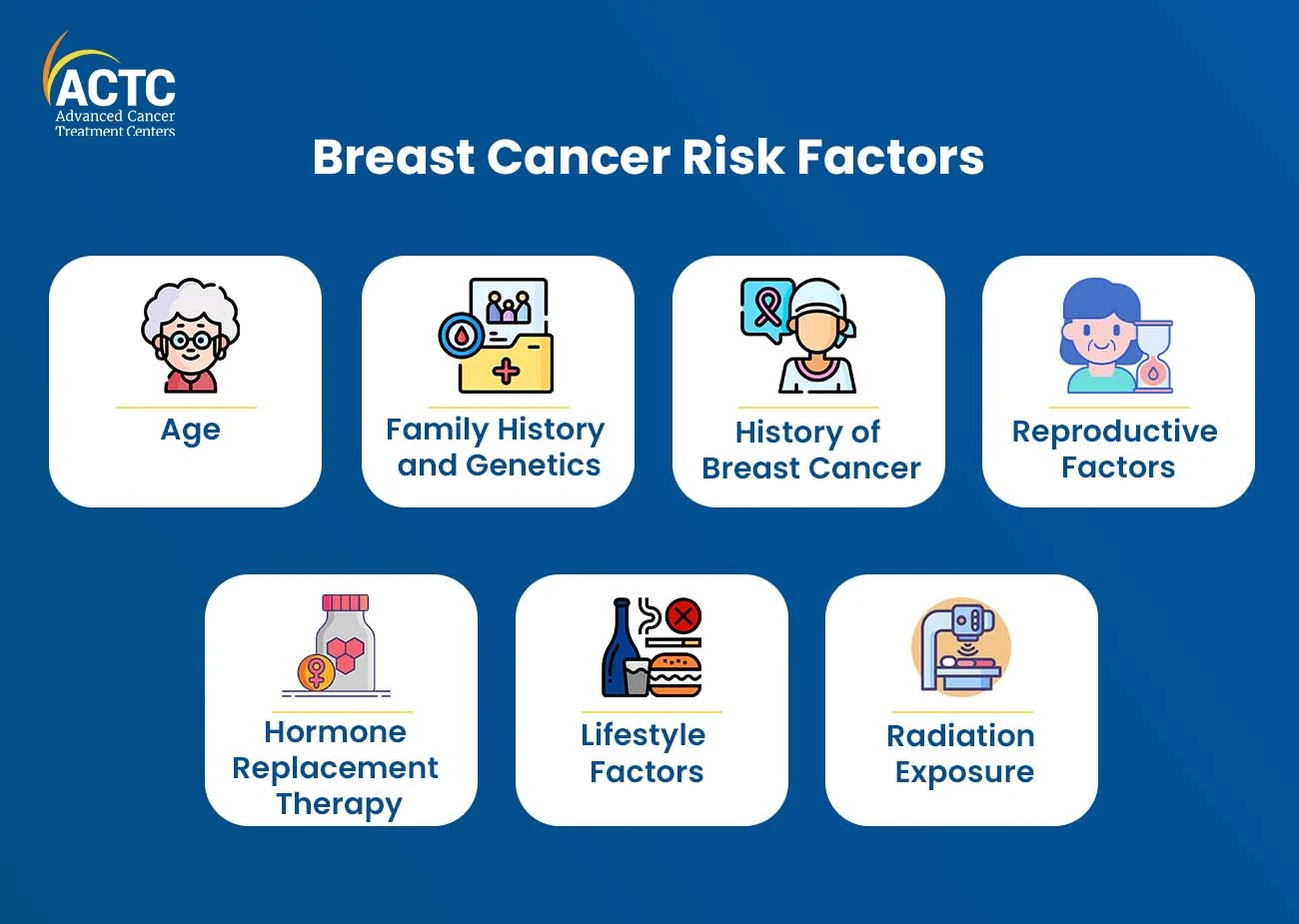
While some risk factors are non-modifiable, such as age and genetics, others are influenced by lifestyle choices and environmental factors.
Key risk factors for breast cancer include:
Age:
The biggest risk factor for breast cancer is getting older. The majority of incidences of breast cancer involve women who are over 50.
Family History and Genetics:
Women with a family history of breast cancer, particularly in first-degree relatives such as mothers, sisters, or daughters, have an increased risk of developing the disease. Additionally, mutations in genes such as BRCA1 and BRCA2 significantly elevate breast cancer risk.
History of Breast Cancer:
Women who have previously been diagnosed with breast cancer or certain benign breast conditions, such as atypical hyperplasia, are at higher risk of developing breast cancer in the future.
Reproductive Factors:
Factors such as early onset of menstruation, late onset of menopause, and nulliparity (never having given birth) are associated with an increased risk of breast cancer.
Hormone Replacement Therapy (HRT):
Long-term use of hormone replacement therapy, particularly combined estrogen-progestin therapy, has been linked to an elevated risk of breast cancer.
Lifestyle Factors:
Modifiable lifestyle factors such as obesity, excessive alcohol consumption, and lack of physical activity can contribute to an increased risk of breast cancer.
Radiation Exposure:
Previous exposure to radiation therapy, particularly during childhood or adolescence, can elevate the risk of developing breast cancer later in life.
Lump or Mass: The presence of a new lump or mass in the breast or underarm area is one of the most common symptoms of breast cancer. While not every breast lump is malignant, each atypical lump must be examined by a medical practitioner as a precaution.
Changes in Breast Size or Shape: Breast cancer may cause one breast to become larger or more misshapen compared to the other breast.
Changes in Breast Skin: Skin changes such as redness, dimpling, puckering, or thickening of the breast skin may indicate the presence of breast cancer.
Nipple Changes: Changes in the appearance or position of the nipple, such as inversion, flattening, or retraction, should be evaluated by a healthcare provider.
Nipple Discharge: While nipple discharge can be caused by various benign conditions, persistent nipple discharge, particularly if it is bloody or occurs only in one breast, should be investigated further.
Breast Pain: Breast discomfort is rarely a sign of breast cancer, but if it persists, a medical practitioner should be consulted.
It is important to note that many of these symptoms can be caused by benign conditions, and the presence of one or more of these symptoms does not necessarily indicate breast cancer.
However, any new or concerning breast changes should be promptly evaluated by a healthcare provider to rule out underlying pathology.
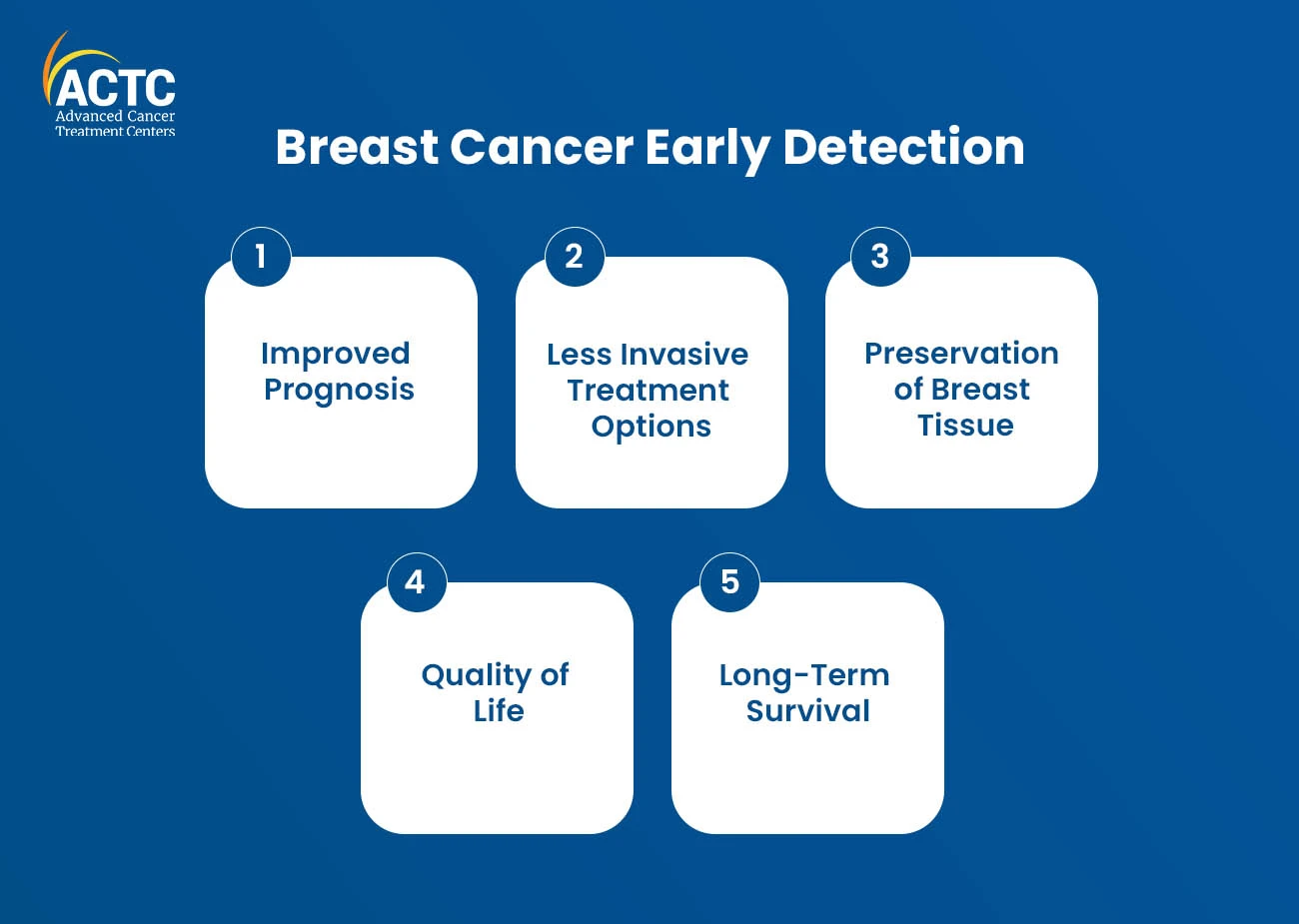
Early detection plays a pivotal role in improving breast cancer outcomes and survival rates. When breast cancer is detected at an early stage, before it has spread beyond the breast tissue, the chances of successful treatment and long-term survival are significantly higher.
Regular breast tumor tests are instrumental in facilitating early detection by identifying breast abnormalities at a stage when treatment options are most effective.
Improved Prognosis:
Early detection allows for prompt initiation of treatment, which can help prevent the spread of cancer to other parts of the body and improve overall prognosis.
Less Invasive Treatment Options:
Early-stage breast cancer may be treated with less aggressive and more conservative treatment approaches, such as lumpectomy (surgical removal of the tumor) or localized radiation therapy, which may result in fewer side effects and a faster recovery time.
Preservation of Breast Tissue:
In some cases, early detection may allow for breast-conserving surgery (lumpectomy) instead of mastectomy (surgical removal of the entire breast), preserving the appearance and sensation of the breast.
Quality of Life:
Early detection can minimize the physical and emotional burden associated with advanced-stage breast cancer, including pain, discomfort, and psychological distress.
Long-Term Survival:
Studies have consistently shown that women whose breast cancer is detected at an early stage have higher survival rates compared to those diagnosed at a later stage.
Regular breast tumor tests are an indispensable component of proactive healthcare for women of all ages. Early detection of breast cancer significantly improves treatment outcomes and enhances overall quality of life.
Connect with ACTC Health, who are pioneers of excellent cancer treatment programs. Schedule an appointment via our website or call us at +1-352-345-4565.
Frequently Asked Questions:
Women with an average risk of breast cancer should begin annual mammograms at age 40. However, individual screening recommendations may vary based on factors such as family history, genetic predisposition, and personal health history.
Clinical breast exams are usually recommended every one to three years for women in their 20s and 30s. After age 40, annual clinical breast exams are often recommended, along with mammograms.
While breast self-exams (BSEs) are no longer recommended as a standalone screening method, they can still complement regular mammograms and clinical breast exams.


January 07, 2026
A chemo port is a small device placed under your skin that makes recei...
KNOW MORE

December 24, 2025
It's natural to wonder if testosterone replacement therapy (TRT) is sa...
KNOW MORE

December 24, 2025
A rash that will not calm down is scary, especially when it changes or...
KNOW MORE
December 24, 2025
Florida’s lung cancer burden remains significant and affects many fa...
KNOW MORE

December 24, 2025
A partial hysterectomy, also called a supracervical hysterectomy, is s...
KNOW MORE

December 24, 2025
Finding a rash on your breast can be unsettling, but remember, many ra...
KNOW MORE
