
Book a Consultation
Thank you!
Your form has been sent successfully.

The pancreas is a pear-shaped gland located between your stomach and spine. It makes enzymes (special proteins) that help your body digest food and hormones like insulin that help control blood sugar levels.
Pancreatic cancer develops when cells in the pancreas change (mutate) and start multiplying uncontrollably, forming a tumor. About 3% of all cancers diagnosed in the United States are pancreatic cancer, and it occurs slightly more often in men than women.
Pancreatic cancers are grouped based on the type of cells where they start. Knowing the type helps doctors determine treatment options and prognosis (the expected outcome).
The two main categories are exocrine cancers and endocrine tumors.
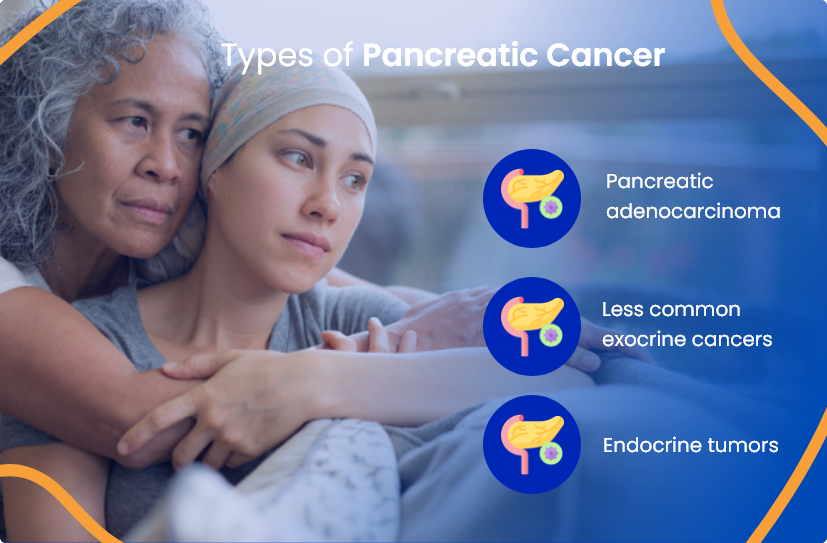
The most common form of pancreatic cancer starts in the exocrine cells, which produce digestive enzymes. About 95% of these exocrine cancers are called adenocarcinomas and begin in tiny tubes (ducts) of the pancreas.
Less common exocrine cancers include adenosquamous carcinoma, squamous cell carcinoma, signet ring cell carcinoma, and undifferentiated carcinomas with or without giant cells.
Pancreatic neuroendocrine tumors (PNETs), also known as endocrine or hormone-related tumors, account for less than 2% of pancreatic cancers.
These tumors can be functioning (making extra hormones) or non-functioning (not making extra amounts of hormones). Examples include insulinoma, glucagonoma, gastrinoma, somatostatinoma, VIPoma, and PPoma.
Pancreatic cancer is often called a "silent disease" because early symptoms are subtle or absent. As it grows, symptoms become more noticeable and can include:
Symptoms vary and often resemble less serious conditions, so discussing ongoing changes with a doctor is important.
To confirm pancreatic cancer, doctors combine physical exams, blood tests, imaging, and biopsies (small tissue samples).
During a physical exam, doctors check for signs of jaundice (yellow skin and eyes) and examine your abdomen for masses or swelling. Blood tests measure bilirubin (a yellow pigment), which may rise if a tumor blocks bile flow.

Imaging helps doctors pinpoint tumor location and size:

A biopsy, often performed through fine-needle aspiration (FNA) or core needle biopsy, collects a small tissue sample from the pancreas. Pathologists examine this under a microscope to confirm cancer cells.
Germline testing (via blood or saliva) checks for inherited genetic mutations that can indicate a higher cancer risk.
Pancreatic cancer treatment is tailored specifically to you, considering your cancer type, stage, potential side effects, overall health, and personal preferences.
Your doctor will discuss the best approach, which may include surgery, radiation therapy, or medication.

Surgery aims to remove the tumor completely, along with a surrounding rim of normal tissue (margin). Depending on the tumor's size and location, surgeons may remove part or all of your pancreas.
The goal is to achieve "negative margins," meaning no cancer cells remain at the edges of removed tissue.
Radiation therapy uses high-energy X-rays or particles to destroy cancer cells by damaging their DNA.
The most common type of therapy for pancreatic cancer is external-beam radiation therapy (EBRT), where the radiation source is a machine outside your body.
Medication-based therapies travel through the bloodstream to treat cancer cells anywhere in your body. Chemotherapy is the most common systemic therapy used for pancreatic cancer.
Targeted therapy and immunotherapy may be used occasionally, especially if your cancer has specific genetic or molecular features.
The cancer specialists at ACTC in Florida deliver personalized, evidence-based care that aligns with your diagnosis, goals, and lifestyle. Our team takes the time to understand your needs and guide you through every step with clarity and compassion.
We’re here to care for the whole person—not just the disease—by supporting both your physical health and emotional well-being throughout treatment and recovery.
The following are our providers whom you can consult at ACTC:

MD, Hematology & Oncology

MD, Ph.D., Hematology/ Medical Oncology

MD, Radiation Oncologist
At ACTC in Florida, our cancer specialists are backed up by qualified clinical staff with over two decades of experience. We guide you through diagnosis, staging, treatment, and long-term follow-up in one convenient location.
Call 352-345-4565 or book an appointment.

ACTC is committed to providing patients with personalized and comprehensive care. A clinical team with over two decades of experience continues to support our caregivers and staff. Our facility features an infusion room, medical and radiation oncology exam rooms, a treatment vault, and cutting-edge diagnostic technology for pancreatic cancer treatment.
Schedule a consultation by calling
 352-345-4565
352-345-4565
Early symptoms of pancreatic cancer are often mild and may resemble less serious health issues. Common warning signs include jaundice (yellowing of the eyes or skin), abdominal pain that radiates toward the back, loss of appetite, unexplained weight loss, digestive issues like nausea, vomiting, or unusual stools, itchy skin, and dark-colored urine. Because symptoms are subtle, it's important to talk to a doctor if they persist.
Smoking is one of the most significant risk factors for pancreatic cancer, roughly doubling the risk compared to non-smokers. While tobacco use substantially increases risk, pancreatic cancer often results from a combination of factors, including genetic predisposition, obesity, and age.
The risk of pancreatic cancer increases significantly with age, and most diagnoses occur in people over age 45, with a higher incidence among those aged 65 and older. Additional risk factors include tobacco use, obesity, type 2 diabetes, chronic pancreatitis (long-term pancreas inflammation), and having a family history of pancreatic cancer or certain genetic conditions.
Schedule a consultation by calling
 352-345-4565
352-345-4565