
Book a Consultation
Thank you!
Your form has been sent successfully.

Immunotherapy is a cancer treatment that uses your body's own immune system to help prevent, control, or eliminate cancer.
Also called biologic therapy, immunotherapy involves treatments derived from living organisms or their lab-made counterparts. It may be used alone or alongside surgery, chemotherapy, radiation, or targeted therapy, depending on your specific cancer and situation.
Immunotherapy helps your immune system fight cancer in two main ways:
 Boost defenses: Stimulates your immune cells, helping them find and attack cancer.
Boost defenses: Stimulates your immune cells, helping them find and attack cancer.
 Add components: Introduces lab-made immune substances that support your body's natural response
Add components: Introduces lab-made immune substances that support your body's natural response
Your eligibility for immunotherapy and the exact approach depend on your cancer type, stage, and overall health.
There are several types of immunotherapy treatments available. Your care team will determine the best option based on your individual cancer and treatment goals.
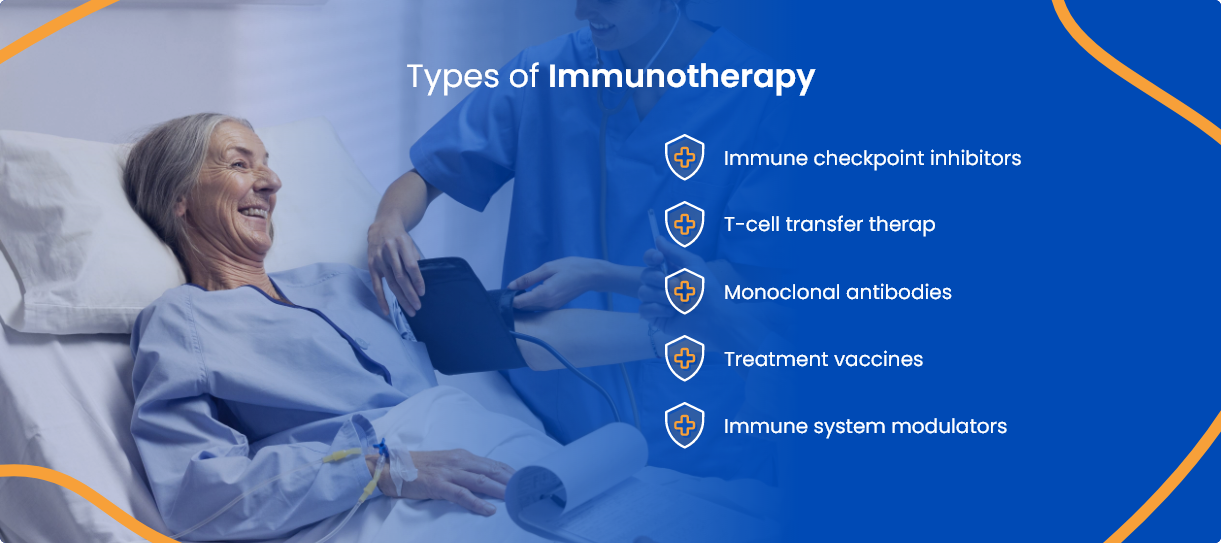

These medications block certain proteins—called checkpoints—that normally prevent immune cells from attacking. By disabling these checkpoints, the treatment helps your immune system recognize and target cancer cells more effectively. Not all patients are eligible for this therapy.

This approach involves collecting your own T-cells, modifying or enhancing them in a laboratory, and then infusing them back into your bloodstream. The goal is to strengthen your immune system’s ability to attack cancer.

Monoclonal antibodies are lab-created proteins designed to bind to specific targets on cancer cells. Some help mark the cancer so the immune system can find and destroy it, while others block signals that allow tumors to grow.

Unlike vaccines that prevent illness, treatment vaccines are administered after cancer has developed. They work by training your immune system to recognize and respond more aggressively to cancer cells, and they may be customized or general

These therapies boost your body’s natural defenses by either targeting specific parts of the immune system or enhancing its overall activity. They help your immune system better detect and attack cancer.
Immunotherapy is commonly administered via IV infusion in an outpatient setting, but delivery methods may vary based on your specific treatment.
How often and how long you'll receive immunotherapy depends on your cancer type, treatment plan, and your body’s response. Ask your care team about the specific type of immunotherapy you will receive and why it’s recommended for you.
Immunotherapy may be considered for treating people with the following types of cancer:
Eligibility for treatment varies based on cancer specifics and personal health. Your care team will help determine whether immunotherapy is appropriate for your situation.
Immunotherapy is a powerful treatment that activates your immune system to target and destroy cancer cells. In doing so, it can also affect healthy tissues, leading to side effects.
The side effects you may experience can vary based on several factors, including your overall health, the type and stage of your cancer, and the specific immunotherapy drug and dose prescribed.
Some of the more common side effects include:
Our cancer care team will walk you through what to expect before treatment begins, but it’s important to monitor any changes in how you feel.
Contact your doctor or nurse if you notice any new symptoms, if existing ones worsen, or if you’re simply unsure whether something is normal. Reporting side effects early gives us the best chance to address them quickly and prevent more serious complications.
In many cases, mild side effects don’t require stopping treatment. We’ll continue monitoring you closely to see how things evolve. If symptoms become moderate or severe, we may pause immunotherapy or prescribe medications to help manage the reaction.
Before starting immunotherapy, ask your care team about:

What type of immunotherapy would you recommend, and why?

What is the main goal of this treatment: cure, control, or comfort?

Is immunotherapy my only option, or will I need additional treatments?

How will the treatment be given to me?

Where will I receive immunotherapy—at your center or somewhere else?

How long does each treatment session take?

How often will I need to come in for treatment?

What are the possible side effects of immunotherapy?

How can I manage any side effects that may come up?

Which side effects should I report right away?

Could the dose or duration of my treatment change over time?

Will I need any scans or tests before, during, or after treatment?

How might this treatment affect my daily life, including work and exercise?

Who can I talk to if I feel anxious or overwhelmed about starting immunotherapy?
ACTC’s cancer specialists in Florida deliver compassionate care tailored to each individual’s needs. Our approach blends evidence-based medicine with emotional support, ensuring a smoother journey for patients and families alike.
You’ll be cared for by a trusted team that includes:

MD, Hematology & Oncology

MD, Ph.D., Hematology/ Medical Oncology

MD, Radiation Oncologist
With decades of combined experience, our team provides comprehensive care—from diagnosis and staging to treatment and survivorship—all in one location.

 352-345-4565
352-345-4565
Schedule a consultation by calling
 352-345-4565
352-345-4565