
Book a Consultation
Thank you!
Your form has been sent successfully.



July 10, 2023
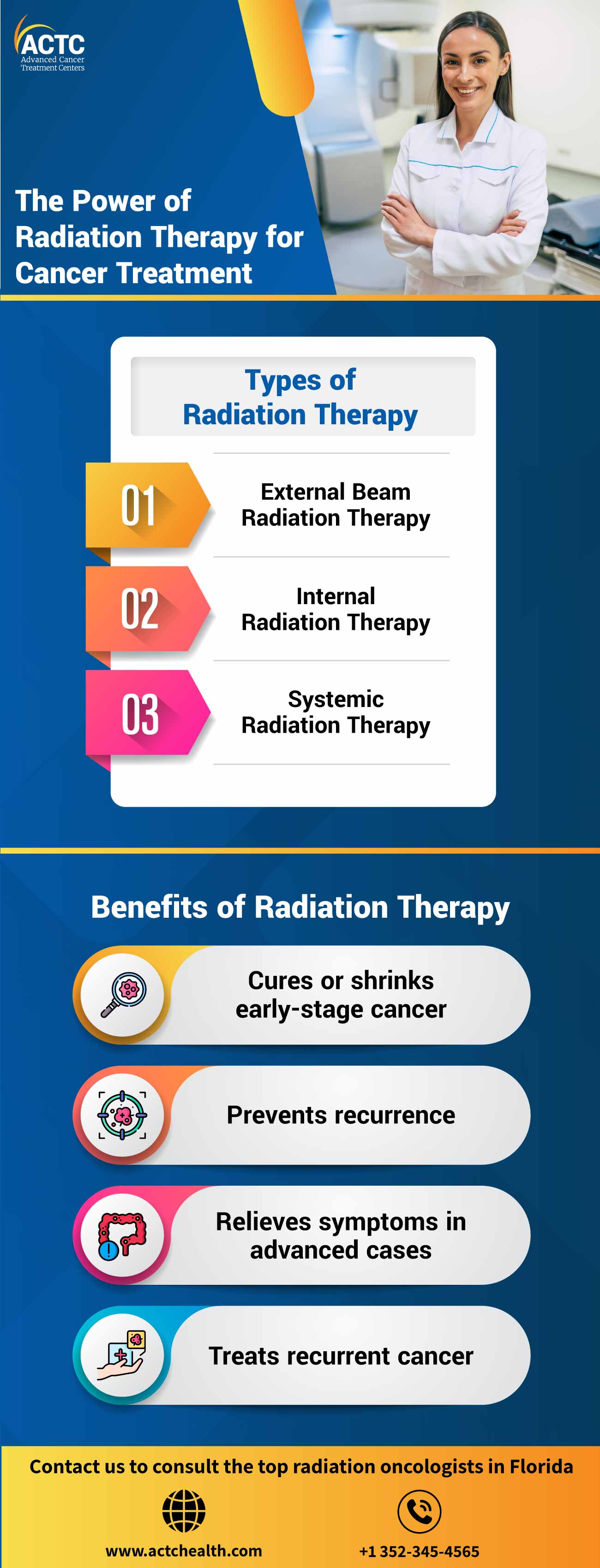
Also known as radiotherapy, radiation therapy is a procedure where oncologists use high-energy radiation to target and kill cancerous cells. It is an integral part of the multidisciplinary approach to traditional cancer treatment, along with surgery and chemotherapy.
In this blog post, we will provide an in-depth understanding of radiation therapy for cancer treatment. We will share detailed information about various aspects of radiation therapy, including different types and techniques, benefits, potential side effects, and recent advancements. Read on to learn more.
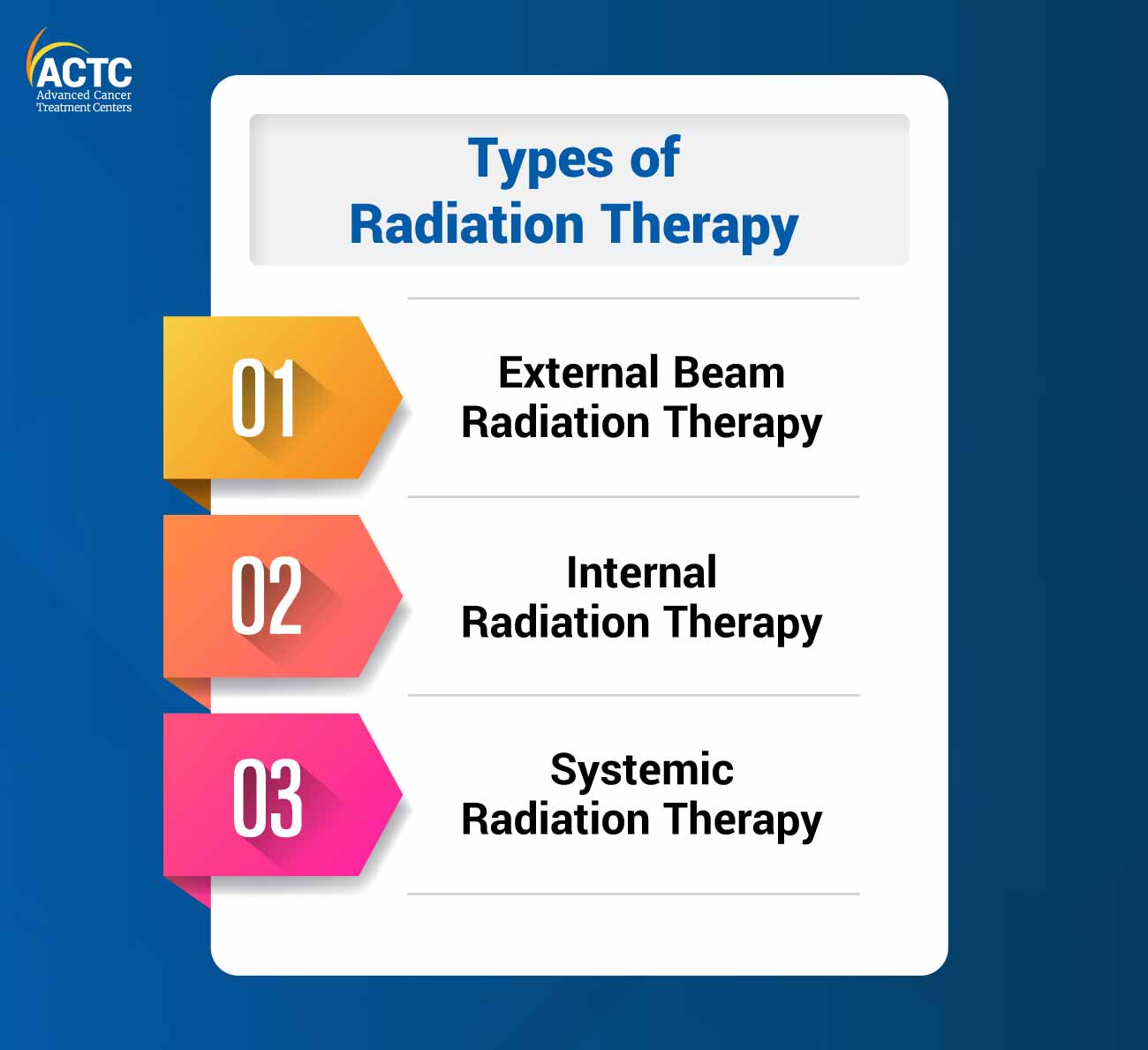
It is the most common form of radiation therapy for cancer, which involves delivering high-energy radiation beams from an external machine directly to the tumor site. The primary goal of this radiotherapy is to target the tumor as precisely as possible in order to save the surrounding healthy tissues.
In EBRT, oncologists utilize advanced imaging techniques, such as computed tomography (CT) scans or magnetic resonance imaging (MRI), to deliver radiation with utmost accuracy.
The following are some subtypes of EBRT:
It involves the use of computer-controlled linear accelerators to deliver radiation from different angles. IMRT enables the modulation of radiation intensity. Therefore, it allows more precise targeting of complex tumors while minimizing radiation exposure to surrounding healthy tissues.
This EBRT technique uses focused radiation beams to deliver a high radiation dose to a specific target and ensures remarkable precision. Cancer care specialists recommend the SBRT technique for treating small tumors or lesions in the brain, spine, lung, liver, and other organs.
This technique incorporates frequent imaging tests during treatment to track tumor position. IRGT ensures precision and minimizes the risk of errors in the treatment caused by organ movements as it adjusts the radiation beams according to the real-time images.
It uses protons instead of photons (X-ray) to deliver radiation therapy. Protons minimize the risk of damage to healthy tissues while they deliver the same radiation dose to the tumor.
Also known as Gamma Knife radiosurgery, this technique uses high doses of focused radiation to destroy small tumors with surgical precision.
This procedure involves delivering radiation during surgery after removing a tumor. IORT helps destroy any remaining cancerous cells which are difficult to remove surgically.
Also known as brachytherapy, internal radiation therapy for cancer involves the placement of radioactive sources internally, directly into or near the tumor. It enhances precision during the delivery of high doses and reduces exposure to surrounding healthy tissues.
The following are two types of internal radiation therapy used in treating cancer:
For this cancer treatment procedure, oncologists place the radioactive sources within body cavities, such as the uterus (intracavitary) or the esophagus (intraluminal). This technique is commonly used in the treatment of gynecological, prostate, and esophageal cancers.
This internal radiotherapy technique involves the insertion of radioactive sources directly into the tumor or the surrounding tissue. It is frequently recommended for treating breast, prostate, and head and neck cancers.
Also known as radiopharmaceutical therapy, this radiotherapy utilizes radioactive substances, which circulate throughout the body to target and destroy cancerous cells. These radioactive substances can be administered orally or intravenously, allowing them to reach cancerous cells wherever they are located. It is commonly used to relieve the symptoms of certain types of thyroid cancer and metastatic bone cancer.
The selection of the most appropriate type of radiation therapy for cancer treatment depends on many factors, including the type and stage of cancer, the location of the tumor, etc. A multidisciplinary team of healthcare professionals evaluates these factors to create a personalized treatment plan depending on individual requirements.
Before internal therapy, individuals typically undergo a physical examination and get imaging tests done.
External beam therapy (EBRT) involves a treatment planning appointment called simulation that helps customize radiation therapy according to individual requirements.
During the simulation, the following steps take place:
Positioning: First, the healthcare provider positions the patient on a table exactly how they will be during the actual treatment sessions. In order to ensure precise alignment, the healthcare team may use a mold or mask to hold the body in place. Then, they may place temporary or permanent markings (tiny dots) to indicate the areas that will receive radiation.
Scans: The patient then undergoes a CT scan or MRI, which provides a detailed image of the tumor’s location. This information assists the healthcare team in customizing the X-rays to precisely target a tumor while minimizing exposure to surrounding healthy tissues.
Internal therapy usually takes place in a specialized outpatient treatment room or a hospital setting. Oncologists may insert the radiation implant using a small flexible tube called a catheter. Before the procedure, providers usually administer anesthesia to ensure a painless procedure. For systemic internal radiation therapy, radioactive fluid is administered through an intravenous (IV) line.
During EBRT, the patient lies on a table, in the same position as decided during the simulation. Then, the machine moves around without making any direct contact. A radiation therapist delivers precise doses to the tumor while adjusting the machine's position. This procedure is usually painless.
Following internal radiation therapy, individuals can generally go home after a brief recovery period on the same day. In rare cases, they may need to stay in the hospital temporarily as the body eliminates trace amounts of radiation. In systemic (IV) therapy, small quantities of radiation may be excreted through bodily fluids such as sweat and urine.
Individuals receiving IV or permanent internal radiation therapy may have a slight risk of exposing others to radiation. Therefore, it is crucial to follow the guidance of the cancer care team regarding the level of contact one should have with others after the session.
In the case of EBRT, individuals can generally resume their daily activities after treatment. There is no risk of exposing others to radiation in external beam therapy.
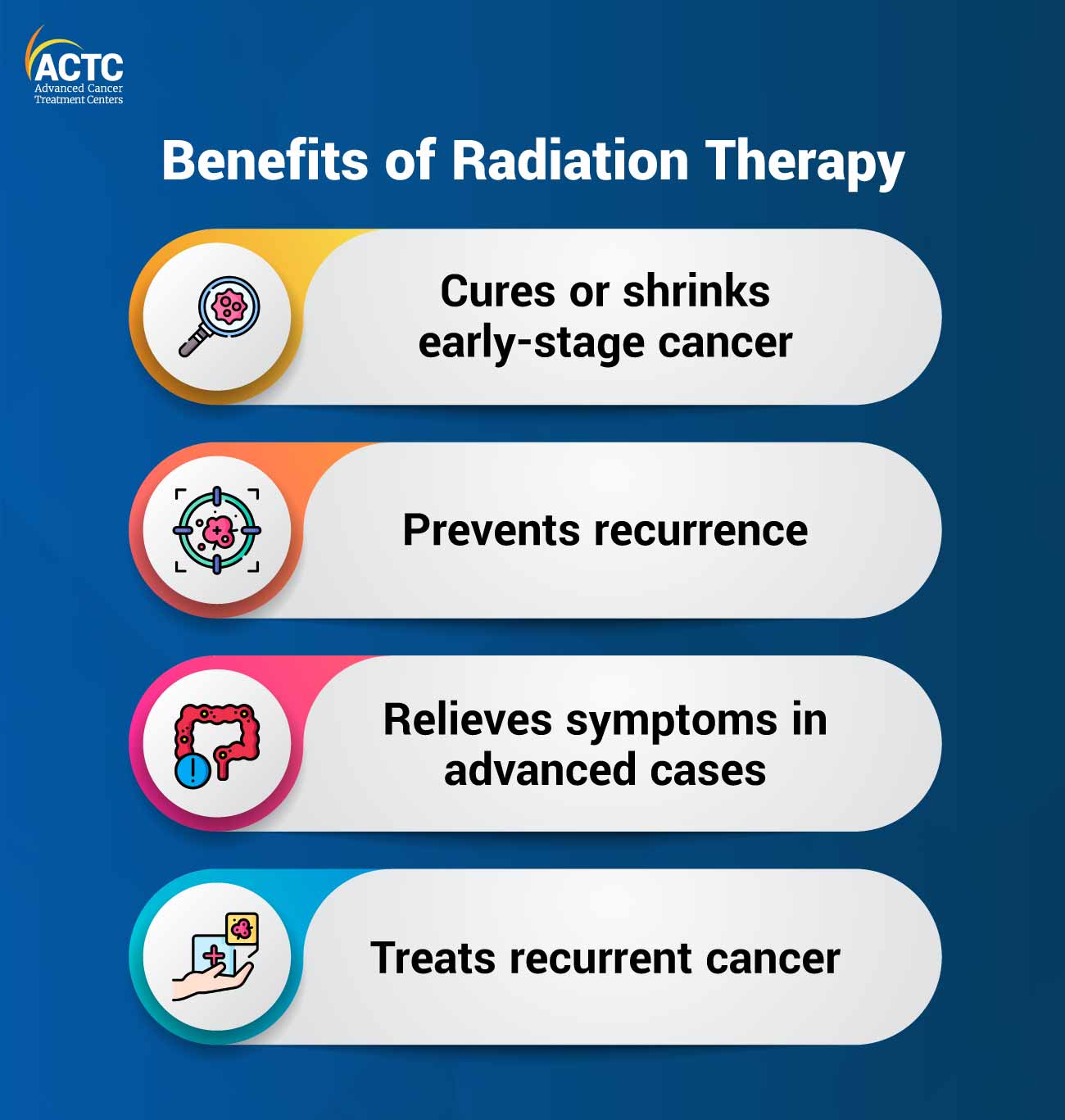
Oncologists often recommend this cancer treatment procedure as the primary treatment for early-stage cancer to make the affected cells shrink or completely disappear. It may be administered before surgery (neoadjuvant therapy) to reduce tumor size or after surgery (adjuvant therapy) to eliminate remaining cancerous cells.
With new technological advancements, oncologists can target specific areas and kill any potential cancer cells. As a result, it prevents recurrence of the disease in those areas.
In advanced cases where cancer has spread extensively and is difficult to cure, radiation therapy can help alleviate symptoms such as pain, breathing difficulties, swallowing problems, or bowel blockages.
If cancer reappears after initial treatment, oncologists may recommend radiation therapy to target the recurring tumor. However, the decision to use this cancer treatment technique again depends on several factors, including the previous dosage and the tumor's response to radiation.
Although radiation therapy is considered an effective treatment option for cancer, it can produce short-term and long-term side effects.
Short-term side effects of radiation therapy are usually visible during treatment and shortly after its completion. These side effects can vary depending on the type of cancer, treatment site, and the individual’s health condition. The following are some common short-term side effects of radiotherapy:
Long-term side effects may develop slowly, often months or even years after treatment. These side effects are generally related to the specific area treated and the cumulative dose. The following are some common long-term side effects of radiation therapy:
Radiation Fibrosis: It is a condition that can cause tissue scarring and stiffness in the treated area.
Chronic fatigue: In some cases, tiredness and exhaustion may persist long after treatment.
In order to manage side effects and enhance well-being during and after radiation therapy for cancer, individuals should communicate with their healthcare team and share any concerns. They not only provide guidance and recommend interventions but also adjust the treatment plan if the symptoms are severe.
Additionally, it is crucial to follow a nutritious diet as recommended by a registered dietitian and drink plenty of fluids. Stay connected with family and friends, join support groups, or get professional counseling services to get emotional support during and after the treatment.
Radiation therapy is a powerful weapon in the fight against cancer, offering remarkable success rates in various cases. It is more effective in the treatment of early-stage cancers, as well as in palliative care.
However, like other cancer treatment procedures, radiation therapy also comes with certain limitations. Cancer care specialists and researchers have shown concerns about potential damage to healthy tissues near the treatment area. Also, the effectiveness of radiation therapy for cancer treatment is limited in advanced cases where cancer has metastasized extensively.
Nevertheless, new technological innovations, such as precision delivery systems and imaging techniques, proton therapy, stereotactic radiosurgery, etc., have further expanded the scope of radiation therapy, enabling more effective and tailored treatments.
For any queries or concerns about cancer treatment, contact ACTC, one of the top cancer centers in Florida, offering individualized cancer treatment plans.


January 07, 2026
A chemo port is a small device placed under your skin that makes recei...
KNOW MORE

December 24, 2025
It's natural to wonder if testosterone replacement therapy (TRT) is sa...
KNOW MORE

December 24, 2025
A rash that will not calm down is scary, especially when it changes or...
KNOW MORE
December 24, 2025
Florida’s lung cancer burden remains significant and affects many fa...
KNOW MORE

December 24, 2025
A partial hysterectomy, also called a supracervical hysterectomy, is s...
KNOW MORE

December 24, 2025
Finding a rash on your breast can be unsettling, but remember, many ra...
KNOW MORE
