
Book a Consultation
Thank you!
Your form has been sent successfully.



November 23, 2022
Skin cancer is highly common in the U.S with melanoma marked as the deadliest form of skin cancer. Melanoma occurrence rates have more than tripled and after having been on the rise for decades.
Despite this, melanoma when detected early is easily curable, hence the key here is – awareness and early detection. The estimated five-year survival rate for patients with early-stage melanoma is around 99 percent in the United States. Therefore, taking steps toward prevention and identification is of paramount importance especially for those with high levels of sun exposure.
The rising percentage of melanoma occurrence is related to several factors including – tanning beds, increase in aging populations and Ozone depletion. Quite a few people are aware of the harmful effects of tanning beds and how they are related to cancer. Research confirms that the extensive use of tanning beds has contributed to the rise in melanoma incidence.
Melanoma is also more common in older adults (65+) possibly due to lack of awareness and the body’s decreased capability to fight mutations with age. An increase in older population also contributes to the rise in numbers as more cases of skin cancer and melanoma are detected.
Certain studies have also linked ozone depletion with melanoma incidence - especially in parts of Australia and New Zealand. With a thinner ozone barrier, people are exposed to higher levels of UV radiation, which can raise the risk of melanoma skin cancer. Because the Antarctic ozone hole is close to Australia and New Zealand, it may explain why skin cancer rates are greater in this part of the planet.
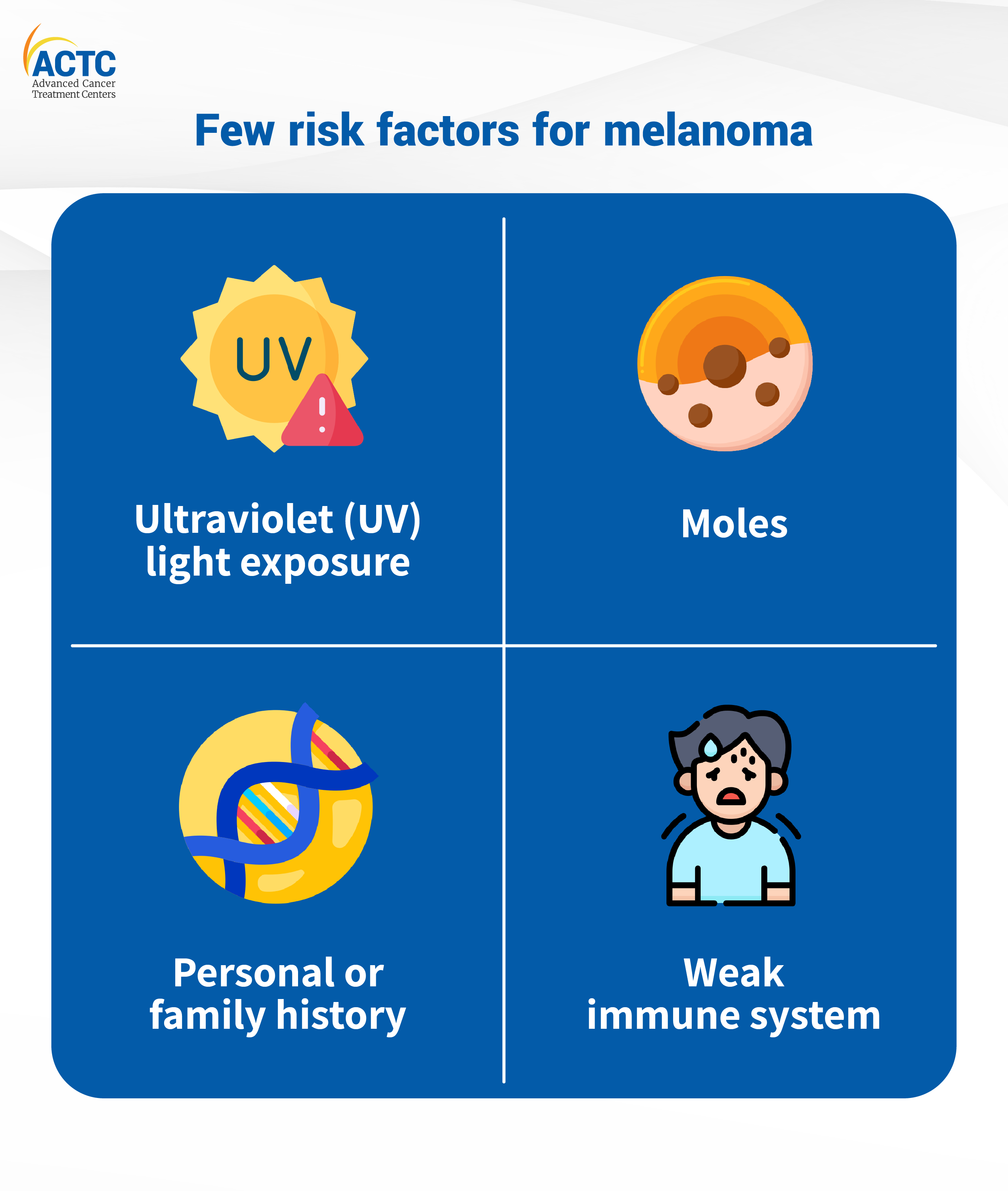
UV light exposure is a primary risk factor for the majority of melanomas. UV rays are mostly emitted by sunlight but artificial sources like tanning beds and sunlamps are also a hotspot for UV rays.
Having a lot of moles: While most moles are harmless, a person with a lot of moles is more likely to get melanoma. Look for moles that grows in size or color or shape.
If one or more of your family members had melanoma, your risk increases. Around 10% of all melanoma patients have a family history of the disease.
People with compromised immune systems (due to specific disorders or medical treatments) are more likely to be at risk.
Everyone's skin is unique. Each of us has a unique pattern of birthmarks, moles, and freckles on our bodies. Fortunately, melanoma often has its own warning signs; here's what to look for in yourself:
Look for asymmetrical moles or growths with an uneven border, color changes, a diameter larger than the size of a pencil eraser, or those that are showing changes in size or thickness. Consult your healthcare physician if you observe one or more of these symptoms.
Melanoma in children and young people does not usually have the same striking black pigmentation as in adults. Pediatric melanoma can take the form of a pink, yellowish, or even white mole or lump or wart-like lesion.
Once you know what to look for, it's crucial to set aside time each month to thoroughly check your skin. Self-examinations are best performed in a well-lit room with full-length and hand mirrors.
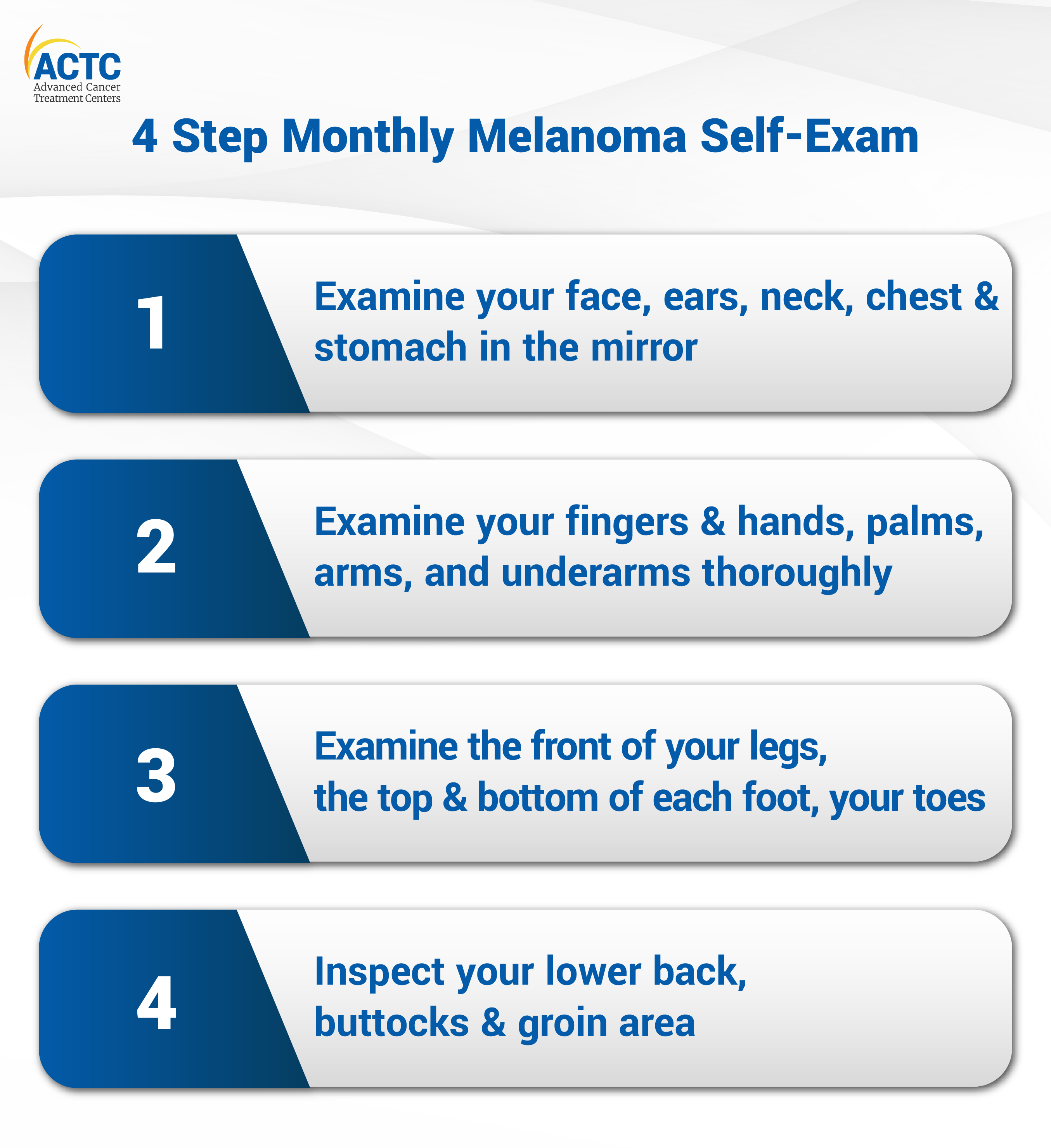
Step 1: Examine your face, ears, neck, chest, and stomach in the mirror. Women should remember to check beneath their breasts.
Step 2: Examine your fingers and hands, palms, arms, and underarms thoroughly. Take a close look at the fronts, backs, and sides of each arm.
Step 3: Examine the front of your legs, the top and bottom of each foot, your toes, and your toenails while sitting. Examine the sides and rear of each leg with a hand mirror. This could also help you see the bottom of your feet!
Step 4: Using your hand mirror, inspect your lower back, buttocks, and groin area. If you're having difficulties seeing everything, try using a combination of full-length and hand mirrors.
In addition to checking your own skin periodically, doctors recommend contacting a dermatologist at least once a year for a comprehensive skin checkup for those at high risk of skin cancer. Do not forget to consult with a dermatologist at least once a year for a comprehensive skin checkup.
People with a personal or family history of melanoma, fair skin, red or blonde hair, light eyes, a history of sunburn/excessive UV radiation exposure, those with many or atypical moles, or a weaker immune system are all at risk for melanoma.
Your dermatologist can assist you in determining how frequently you should get a full-body skin inspection based on your unique risk factors.
Dermatologists are specially trained to diagnose skin cancer, including melanoma, at an early stage. To examine moles more closely, many doctors will use a dermascope, which combines a flashlight and a microscope. They may even photograph moles in order to monitor them over time. If a dermatologist notices something unusual, it will be biopsied for additional examination.
As you become more comfortable inspecting your skin, you'll develop a clear picture of your body and its moles. This is especially helpful as you can easily spot any changes in the future. Also, do not hesitate to consult a dermatologist if you find abnormalities anywhere in the body.
Start your skin care journey today by reducing exposure to sun and taking monthly skin exams.


January 07, 2026
A chemo port is a small device placed under your skin that makes recei...
KNOW MORE

December 24, 2025
It's natural to wonder if testosterone replacement therapy (TRT) is sa...
KNOW MORE

December 24, 2025
A rash that will not calm down is scary, especially when it changes or...
KNOW MORE
December 24, 2025
Florida’s lung cancer burden remains significant and affects many fa...
KNOW MORE

December 24, 2025
A partial hysterectomy, also called a supracervical hysterectomy, is s...
KNOW MORE

December 24, 2025
Finding a rash on your breast can be unsettling, but remember, many ra...
KNOW MORE
