
Book a Consultation
Thank you!
Your form has been sent successfully.


December 24, 2025
Florida’s lung cancer burden remains significant and affects many families, and hearing “you may need your whole lung removed” can stop you in your tracks.
We understand that this can raise questions about breathing, hospital time, and returning to normal near home.
Our goal is to provide clarity. To do that, let’s discuss pneumonectomy, who may need it, key risks, and how recovery works.
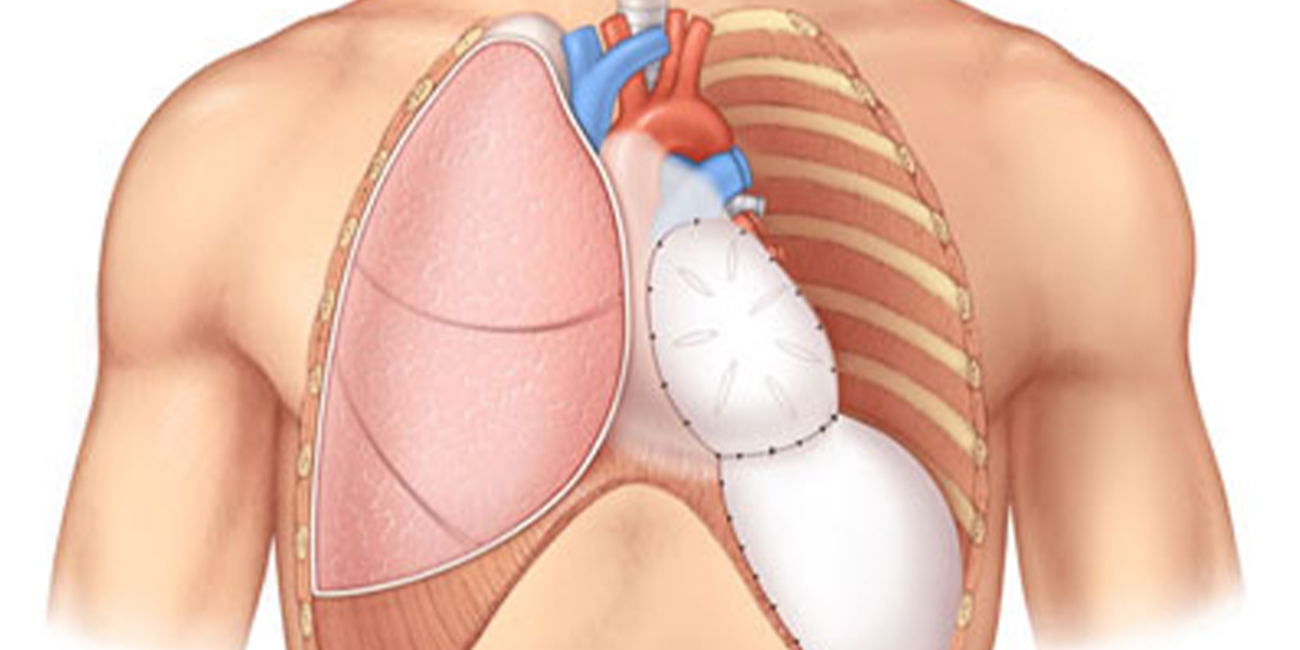
Pneumonectomy is surgery to remove one entire lung—the right or the left—when a smaller operation cannot safely clear the disease. Fortunately, many people can live an active life with one lung after recovery and training.
A pneumonectomy is considered for central lung cancers that involve a main airway, certain mesotheliomas, and some badly damaged or infected lungs when function can’t be saved.
When discussing the procedure, you may also hear related terms:
Below are the different types of pneumonectomy procedures your doctor may consider:
| Type | When considered | Key notes |
|---|---|---|
| Simple pneumonectomy | Central tumor without chest wall spread | Standard whole-lung removal |
| Sleeve pneumonectomy | Tumor involves main airway and vessel | Airway reconstruction |
| Extrapleural pneumonectomy | Select mesothelioma cases | Lung, lining around lung, pericardium, and part of diaphragm removed |
| Completion pneumonectomy | Prior major resection on same side | Higher risk; careful selection |
| Right vs left | Depends on anatomy and disease | Right side often has higher physiologic impact |
Major risks after pneumonectomy include:
Right-sided pneumonectomy generally carries a higher risk than left-sided because of anatomy and blood-flow differences.
Enhanced Recovery After Surgery (ERAS) pathways lower complications and can shorten the stay. These include good pain control, early walking, and careful fluids.
A safe plan starts with accurate staging and fitness testing. We check pulmonary function tests (PFTs) and often use a perfusion scan to see how much work the diseased lung is doing.
When numbers are borderline, a cardiopulmonary exercise test measures how your heart and lungs perform together.
We avoid surgery if cancer has spread outside the chest or if heart-lung reserve is too low (such as severe pulmonary hypertension). You can improve safety to reduce complications and speed recovery by:
If pneumonectomy is advised, selection is careful. We look at your scans, lung tests, heart health, and goals.
Most patients have an open approach through a thoracotomy. The first day or two are watched closely for breathing, heart rhythm, and fluids. We also discuss risks and the expected hospital course before any decision.
Radiation can help when surgery is not safe or as part of a plan before or after surgery, depending on the cancer’s stage and margins. Your plan aims to control the disease while protecting the remaining lung.
Systemic therapy—chemotherapy, immunotherapy, or targeted therapy—may be used before or after surgery based on stage and tumor markers.
The goal is to lower the chance of cancer returning and to treat any cells that have traveled.
Our top-center-trained oncologists coordinate complex thoracic care locally, so decisions and treatments align with current national standards while staying close to home.
Most patients spend the first 24–48 hours in the intensive care unit so we can monitor breathing, heart rhythm, and blood pressure closely.
The typical hospital stay is about six days when recovery is smooth. After the procedure, pain control is a priority. An epidural catheter or a nerve block can reduce pain, help you breathe deeply, and lower the risk of pneumonia.
Walking early, eating early, and careful fluid management are parts of “enhanced recovery” pathways.
Some patients go home with oxygen. Many can wean off over the next weeks to months as the remaining lung gets stronger.
You can ask your doctor when you’re cleared for other activities, such as:
Call us right away if you notice:
After your procedure, expect frequent visits and chest CT scans for the first two years, then gradually less often. Many people return to a good daily routine—walking, light chores, time with family—though long-distance walks or heavy lifting may feel different.
Pulmonary rehab improves endurance and confidence. If you work, desk jobs may resume in 6–8 weeks; physically demanding jobs often take longer and may need adjustments.
For further questions, you can call 352-345-4565 or book an appointment.


January 07, 2026
A chemo port is a small device placed under your skin that makes recei...
KNOW MORE

December 24, 2025
It's natural to wonder if testosterone replacement therapy (TRT) is sa...
KNOW MORE

December 24, 2025
A rash that will not calm down is scary, especially when it changes or...
KNOW MORE

December 24, 2025
A partial hysterectomy, also called a supracervical hysterectomy, is s...
KNOW MORE

December 24, 2025
Finding a rash on your breast can be unsettling, but remember, many ra...
KNOW MORE
December 16, 2025
Hearing a HER2 gene mutation on a report can feel scary, but it also p...
KNOW MORE
