
Book a Consultation
Thank you!
Your form has been sent successfully.



January 07, 2026
A chemo port is a small device placed under your skin that makes receiving chemotherapy drugs and blood draws safer and easier. It isn't permanent; it's used only as long as needed, often for months to years, and then removed.
Our team understands your worries and follows current national guidelines to individualize your choice. We'll clearly explain what a chemo port is, when it's recommended, and exactly what to expect at each step, right here in Brooksville.
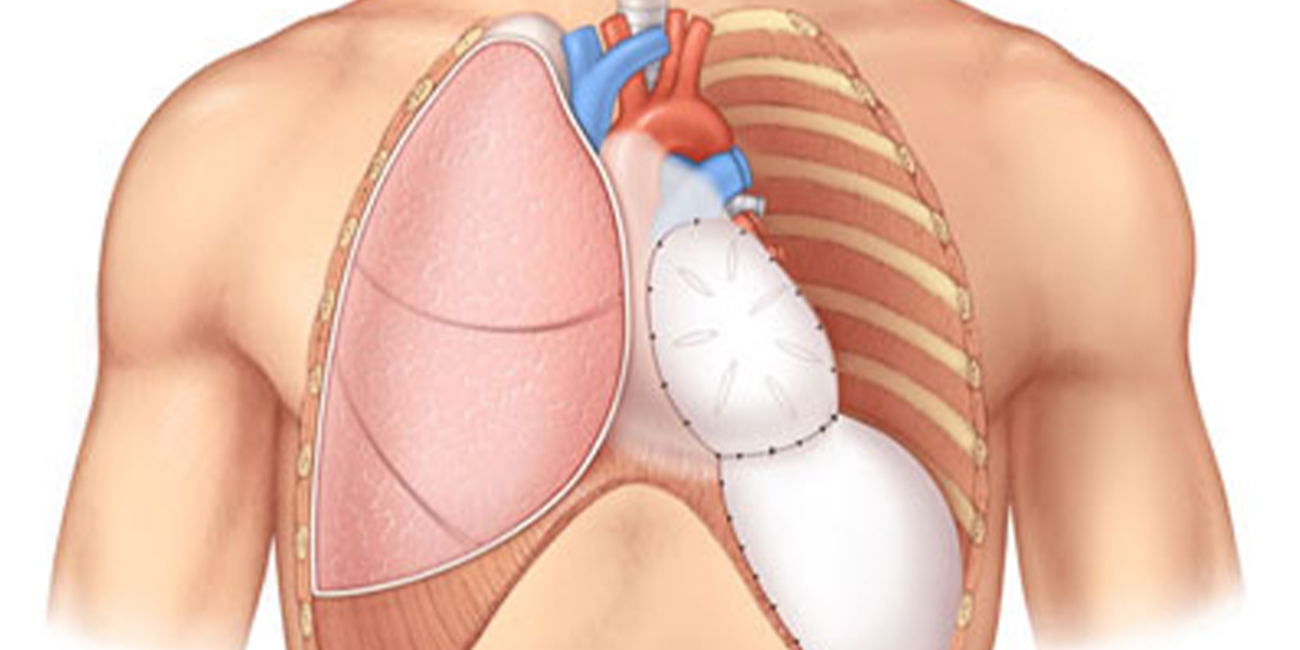
A chemo port, or implanted port, is a small, round or triangular reservoir (about the size of a quarter) placed beneath your skin, typically in your chest or upper arm. A thin, flexible plastic tube (catheter) connects this reservoir directly to a large vein near your heart.
When you need chemotherapy or blood draws, your nurse accesses the port by placing a special non-coring needle (Huber needle) through your skin into the port’s reservoir. The port can be accessed repeatedly because this needle doesn't damage the silicone cover (septum).
Ports often have one channel (single-lumen), suitable for most patients, though some have two (double-lumen) for special cases.
Many newer ports are "power-injectable," meaning they're safe for the high-pressure contrast used in CT scans.
You can also fly safely with a port. Screening is usually straightforward, but some implants may trigger detectors. Inform TSA officers and consider carrying a medical notification card.
If you're comparing venous access options, here’s a helpful overview of common devices used in cancer treatment:
| Device | Where Implanted | Use Duration | Pros | Cons | Typical Users |
|---|---|---|---|---|---|
| Port (Implanted Port) | Chest or upper arm under skin | Months to years | Hidden under skin; minimal daily care | Minor surgery needed | Frequent or long-term chemotherapy |
| PICC Line | Upper arm vein | Weeks to months | No surgery required | External line needs regular care | Intermediate-length treatments |
| Tunneled Catheter | Chest vein | Months | Provides high-flow access | External catheter; higher infection risk | Complex, frequent access needs |
| Midline Catheter | Arm vein | Weeks | Easy, fast placement | Limited medication use | Non-vesicant IV treatments |
| Peripheral IV | Hand or forearm | Hours to days | Quick and easy | Vein irritation; frequent replacements | Short-term or one-time treatments |
Chemo port placement is usually a quick outpatient procedure performed under local anesthetic (numbing medication) and mild IV sedation (medicine to help you relax).
Your ACTC surgeon or interventional radiologist will use ultrasound guidance to precisely insert the catheter into a vein, typically in your chest or arm. After the catheter is positioned, they'll confirm correct placement with a chest X-ray or fluoroscopy (live X-ray).
You might experience mild soreness, tenderness, or bruising around the port site for a few days. Most patients return to non-strenuous daily activities or office work within 1 to 3 days after placement. Heavier lifting and strenuous exercise should wait about 1 to 2 weeks to ensure proper healing.
Here are some simple self-care steps after port placement:
A chemo port must always be accessed using a special non-coring needle called a Huber needle. Our infusion nurses will follow strict sterile procedures each time to protect you from infection.
Before administering chemotherapy, IV fluids, or drawing blood, the nurse ensures your port is working properly by confirming smooth flushing and good blood return.
If your port remains accessed continuously for treatment, the needle and dressing will be changed at least every 7 days. When your port isn’t in regular use, our guidelines recommend flushing it every 4–12 weeks (typically about every 6–8 weeks) to maintain its function and prevent clotting.
Call ACTC right away if you experience:
All venous access devices have some risks. The two most common are infections and blood clots (deep venous thrombosis). Compared to external devices like PICC lines, ports generally have lower risks of both.
At ACTC, we use ultrasound guidance during placement, follow strict sterile protocols, regularly inspect your port site, and adhere to evidence-based flushing procedures to minimize these risks.
If a clot blocks your port, medication can often clear it. Infections, though rare, are managed swiftly with antibiotics and sometimes the removal of the device.
Conditions such as active infections, bleeding disorders, or previous blood clots require careful evaluation. Our team carefully assesses each patient to minimize complications.
After your incision heals (usually around two weeks), your port won't limit most daily activities, such as showering. When your port is not accessed, swimming is generally allowed. However, follow your care team’s advice and avoid soaking until cleared.
When accessed, keep the area dry and avoid soaking it in water. Traveling by plane with your port is safe, and it rarely sets off airport security detectors.
Still, carrying your medical device card helps explain things smoothly during screening. Many newer ports are "power-injectable" and safe for CT scan contrast. Most ports are MR-Conditional (or MR-Safe); radiology will confirm your device model and any scan conditions before your scan.
Choosing a venous access device is a decision you and your healthcare team make together. At ACTC, your medical oncologist, surgeon, and interventional radiologist will carefully evaluate your chemotherapy regimen, vein condition, infection risk, and personal lifestyle before recommending the best option.
If you're receiving chemotherapy drugs that could harm small veins (vesicants), need frequent IV treatments or blood draws, or anticipate long-term therapy, we usually recommend a chemo port. For shorter treatments or immediate access needs, a PICC line or peripheral IV might be enough.
At ACTC, top-center-trained oncologists coordinate these decisions, ensuring you're comfortable and informed. Our in-house infusion center offers the added convenience of tele-oncology follow-ups when appropriate.
Chemo ports provide significant advantages for adults undergoing long-term chemotherapy, especially treatments that are frequent or involve medications that could irritate or damage smaller veins.
Seniors often prefer ports for their convenience and reduced risk of complications. Immunocompromised patients also benefit due to the lower infection risks compared to external lines.
If you're on blood-thinning medications, we'll work closely with your care team to safely schedule your port placement. For pediatric patients, decisions about ports are carefully made with specialized pediatric oncology teams to ensure safety and comfort.
At ACTC, every patient receives personalized guidance on choosing the most suitable device to meet their treatment goals and lifestyle. Call 352-345-4565 or book an appointment now.


December 24, 2025
It's natural to wonder if testosterone replacement therapy (TRT) is sa...
KNOW MORE

December 24, 2025
A rash that will not calm down is scary, especially when it changes or...
KNOW MORE
December 24, 2025
Florida’s lung cancer burden remains significant and affects many fa...
KNOW MORE

December 24, 2025
A partial hysterectomy, also called a supracervical hysterectomy, is s...
KNOW MORE

December 24, 2025
Finding a rash on your breast can be unsettling, but remember, many ra...
KNOW MORE
December 16, 2025
Hearing a HER2 gene mutation on a report can feel scary, but it also p...
KNOW MORE
